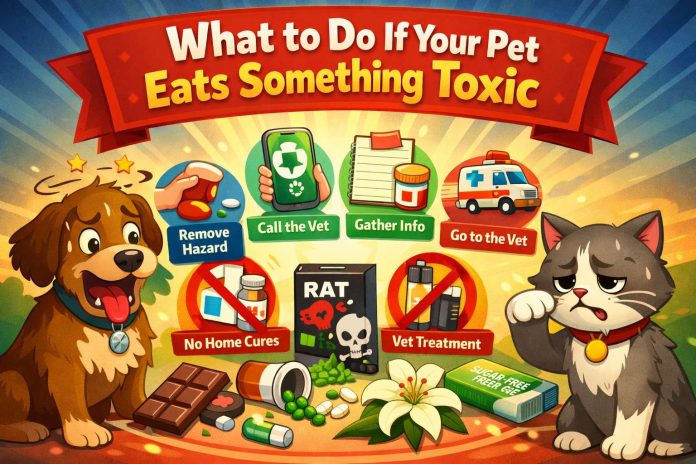
It happens fast. One second your pet is fine, and the next they are chewing something they should never touch. A dropped pill, a cleaning pod, a sugar-free snack, or a random plant leaf can turn into a real emergency.
So, take a breath. Then act. The goal is simple. Stop the exposure, get the right info, and call the right help line as soon as you can.
Below is a step-by-step plan that works for most situations. It is practical, and it keeps you focused when your brain wants to freeze.
Step 1: Stop access right now
First, move your pet away from the area. If they still have the item in their mouth, take it out carefully. Then pick up any crumbs, spilled liquid, or broken pieces. After that, put the product in a sealed bag or container.
Next, block off the room if needed. Pets love to go back for “one more taste,” so you want the danger out of reach.
Step 2: Check breathing, alertness, and body control
Now look at your pet for urgent red flags. These signs mean emergency care right away:
- Trouble breathing
- Collapse or extreme weakness
- Seizures
- Uncontrolled shaking
- Blue, gray, or very pale gums
- Fast swelling of the face or muzzle
- A hard, swollen belly with distress
If you see any of these, do not wait. Instead, head to the nearest emergency clinic.
Step 3: Identify what was eaten, and estimate the amount
Next, figure out what your pet got into. Grab the packaging and take a clear photo of the front label and ingredient list. Then write down these details:
- Product name
- Strength or dose (for medicine)
- Time of exposure
- Amount missing
- Your pet’s weight
This part matters more than people think. A vet can only make fast decisions if the facts are clear. Even a rough estimate helps.
Step 4: Call a veterinarian or an animal poison hotline
Then make a call. Pick the fastest option you can reach:
- Your regular vet
- A local emergency veterinary hospital
- ASPCA Animal Poison Control Center (24/7)
- Pet Poison Helpline (24/7)
After you connect, share your notes and photos. Then follow the instructions exactly. That plan will match the toxin, the timing, and your pet’s size.
If you want a quick reminder of common household dangers, read this guide on hidden pet killers at home. It covers everyday items many owners still overlook.
Step 5: Skip home “cures,” and do not force vomiting
At this point, it is tempting to do something dramatic. That urge is normal. Still, many home fixes backfire.
So, do not give milk, oil, salt water, or random “detox” mixes. Also, do not use activated charcoal unless a vet tells you to. And do not use hydrogen peroxide unless a vet gives you the exact dose and confirms it is safe.
Vomiting is not always the answer. Some products burn the throat on the way back up. Other toxins raise the risk of choking or breathing vomit into the lungs. So, wait for professional guidance before you try anything at home.
Step 6: Get ready to leave for the clinic fast
If the vet says “go now,” then go. Pack what helps them treat your pet quickly:
- The product packaging or bottle
- A piece of the plant or bait (sealed)
- Chewed parts, batteries, wrappers, or pills
- A sample of vomit or diarrhea (sealed, if you can do it safely)
Next, keep your pet calm and contained. Use a carrier for cats and small dogs. Use a leash for dogs, even inside the waiting room. Then keep the car cool and quiet.
Step 7: Watch for delayed symptoms for the next 24 hours
Some toxins hit hard right away. Others take hours. So even if your pet looks “okay,” stay alert during the next day.
Watch for:
- Vomiting or diarrhea
- Drooling or pawing at the mouth
- Sudden tiredness
- Stumbling or confusion
- Refusing food
- Yellow gums or eyes
- Bloody stool
- Rapid heart rate
Then write down what you see and when it starts. That timeline helps the vet spot patterns faster.

“Should I wait for symptoms?” Usually, no
This is a common question, and the honest answer is simple. Waiting can waste the best treatment window.
Many toxins cause damage before the signs look scary. So, if you know your pet ate something risky, call right away. Even if your pet seems normal, the vet may still recommend monitoring, lab work, or early treatment.
Common toxins that surprise pet owners
A lot of pet poisoning comes from normal household items. So, here are the big categories that show up again and again.
Human medications
First, human meds can be dangerous even in small amounts. Pain relievers, antidepressants, sleep aids, and cold remedies can all trigger serious symptoms. So, store every bottle behind a closed door, not on counters or nightstands.
Sugar-free foods and dental products
Next, xylitol is a sweetener found in many sugar-free products. Dogs can develop a dangerous drop in blood sugar after exposure. In some cases, liver injury follows. So treat any xylitol exposure as urgent.
Chocolate, caffeine, and nicotine
Then there are the “snack” toxins. Chocolate risk depends on type, and dark chocolate is usually worse than milk chocolate. Caffeine and nicotine can trigger tremors, heart problems, and seizures too. So, call as soon as you suspect exposure.
Rodent bait and insect bait
After that, bait products can be tricky. Some cause internal bleeding. Others cause seizures. So packaging really matters, since different baits need different treatment.
Cleaning products and chemicals
Cleaning pods, bleach, drain cleaners, and antifreeze can cause serious injury. Some burn the mouth and throat. Others harm organs. So do not delay if your pet licks or drinks a chemical.
Batteries and magnets
Button batteries can burn tissue fast. Magnets can damage the intestines in a very dangerous way. So, treat these as emergencies, even if your pet acts normal at first.
Toxic foods for cats
Cats have their own “kitchen danger list.” Some foods cause stomach upset, and some can harm organs. If you have a cat at home, this guide on foods cats should never eat is a useful one to keep bookmarked.
What a vet may do at the clinic
Once you arrive, the vet picks treatment based on the toxin and the timing. That can include:
- Medicine to stop vomiting
- IV fluids for hydration and organ support
- Blood tests to track liver, kidney, and electrolytes
- Imaging for batteries, sharp objects, or magnets
- Professional charcoal treatment in select cases
- Hospital monitoring for heart rhythm, glucose, or seizures
In many cases, early care means fewer complications. It can mean fewer days of monitoring too.
A quick prevention checklist for today
You can reduce risk with a few habits:
- Store meds, vitamins, and supplements behind a closed door
- Keep gum, mints, and sugar-free snacks out of reach
- Use a lidded trash can, and keep it in a closed room
- Do not leave bags on the floor, even for a minute
- Keep cleaning supplies in a high cabinet
- Skip lilies in homes with cats
- Use bait only in secure stations, never loose
Then save your vet’s number and your nearest emergency clinic in your contacts. It sounds basic, but it saves time when it counts.